

In this
issue

WELCOME
NURSING SCIENCE
EDUCATION
PRACTICE

Does Using the "4M's Framework: What Matters Most" Improve Patient Satisfaction?

Mary E. Mahoney Simulation Center
PROFESSIONAL DEVELOPMENT
FROM OUR TEAMS

EKG Puzzler

The Importance of Patient Satisfaction at the Bedside

PCA Academy

Patient Safety, Satisfaction & the UAA

ABOUT DISCOVERN
PRACTICE
Does Using the "4M's Framework: What Matters Most" Improve Patient Satisfaction?
By: Shawntay Fernandez, BSN, NE-BC, Citadel Rafols, MSN, CMSRN and Thelma Ekezie, BSN, RN
By: Shawntay Fernandez, BSN, NE-BC, Citadel Rafols, MSN, CMSRN and Thelma Ekezie, BSN, RN
4 MIN READ

Patient satisfaction is an integral part of the Houston Methodist healthcare delivery system that can also help improve patient outcomes. As a result, improving patient satisfaction scores has become a priority for the Dunn 10 East team, which cares for liver and gastrointestinal patients.
Changes in the healthcare system and the emergence of the pandemic have made it more challenging to increase patient satisfaction. The pandemic changed healthcare in ways we could have never imagined. The healthcare team is required to wear masks and shields during every patient interaction, which makes patient care difficult and less personal. In addition, visitors were limited, which isolated the patient even further. In an attempt to strengthen patient-centered care, the team looked at reinforcing the fundamentals of nursing care, specifically compassionate, individualized, and in-the-moment care. We looked for methods that promote sustainable change and incorporate evidence-based practices within the unit and allowed us to align optimal care with each patient's goals and unique preferences. This led to a collaboration with Dr. Kathryn Agarwal, the Medical Director of Post-Acute Care for the Houston Methodist Coordinated Care Program and the Chair of the System Delirium Committee, in the pursuit of our goal for Houston Methodist Hospital to be recognized as an Age-Friendly Health System and to improve patient satisfaction. We are fortunate enough to have Dr. Agarwal and our unit leaders, Susan Teer and Shawntay Fernandez, who provided us with the foundation and guidance that made this initiative successful.
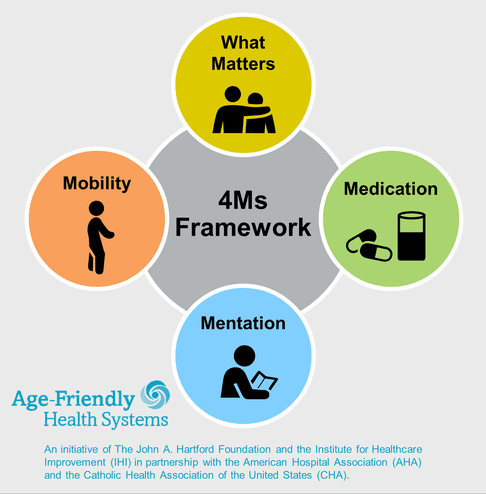
The John A. Hartford Foundation and the Institute for Healthcare Improvement (IHI), in partnership with the American Hospital Association (AHA) and the Catholic Health Association of the United States (CHA), have established criteria and expectations of health care organizations to meet the needs of the growing elderly population. The Age-Friendly Health System initiative encourages using a set of evidence-based practices to cause no harm and consider what matters to the older adult and their family caregivers. This initiative consists of providing a set of four evidence-based elements of high-quality care, known as the "4Ms," to all older adults.
Using the 4Ms Framework and focusing on What Matters, we were able to tailor our care using the question: "What is most important to you today?" This allowed us to prioritize the patients' needs and change our patient care perspective by asking the following questions. What is most important to the patient when they are not at their optimal state of health? When might they be most vulnerable? How can the patient feel that their needs are being addressed and prioritized? Through our collaboration with Dr. Agarwal, Dunn 10 East set off on a journey to find out what mattered most to our patients.
Through these questions, we hoped to align the patient's goals with their care. The nurses asked these questions during admission. The staff used the information obtained from the "Get to Know Me" questions to individualize care and motivate patients to achieve their goals. For example, Mr. Smith likes to go fishing, so his nurse encouraged him to get up and walk so that he may be able to return to fishing after discharge. Our leaders performed audits using the My Rounding Template and talked to patients during leadership rounding to monitor compliance. Following the three-month pilot study, our HCAHPS results were reviewed; however, our patient satisfaction scores did not increase as we expected. A post-implementation survey was performed. Staff responses to the pilot study were encouraging as the nursing staff noted positive influences since the implementation of the pilot. We decided to momentarily pause the pilot while we moved to a different unit and collaborated with Dr. Agarwal once again to come up with a reboot to our original pilot. The "Get to Know Me" reboot, now referred to as "What Matters Most" pilot kicked off with a few changes. Nurses were no longer asking the patients three questions, but rather a single question daily: "What's the most important thing we can do for you today?" Those responses were updated on the whiteboard daily.
As a unit, we were excited to implement a method that we believed would showcase our desire to improve the patient care experience. We called this initiative "Get to Know Me." Dr. Agarwal presented the background of the 4M's Framework and the desire of the hospital to achieve the Age-Friendly designation to the staff. A survey was done before implementing the project to get the baseline data on how well we know our patient's preferences and goals. Through collaboration with Dr. Agarwal and her team, three questions were chosen to ask the patient to determine what mattered most to them. Those questions were:
• "my preferred name",
• "my favorite activity", and
• "When I leave the hospital, I am looking forward to?"
Additionally, the patients were asked how they preferred to be addressed. Our goal was to tailor patient care based on what was important to them that day. Patients' responses ranged from taking a shower to getting them through a liver transplant and somewhere in between. Similar to the original pilot, leadership rounded on patients to monitor compliance. During the leadership rounds, patients expressed that what mattered to them was being prioritized.
The patients' satisfaction was reflected in our HCAHPS scores following implementation. Dunn 10 East has seen an increase in patient satisfaction survey scores, moving from an overall HCAHPS score of 78.5 % for 2020 to 83.6% in the year to date. Furthermore, communication with nurses scores also increased on the HCAHPS survey from an overall score of 75.4% in 2020 to 81.8% in the year to date.
Based on our preliminary results, using the "What Matters Most" element of the 4Ms Framework has increased our patient satisfaction outcomes. As we continue to advance the patient care experience, we are excited to continue implementing this initiative. In doing so, it is our wish as a unit to personalize patient care and continue asking our patients what is most important to them.
References:
Related Articles
EDUCATION
Barcode Specimen Scanning
PROFESSIONAL DEVELOPMENT
Preceptor Academy Has Launched!
Contact us at CNREPHelp@houstonmethodist.org
Questions or comments?
© 2021. Houston Methodist, Houston, TX. All rights reserved.







