

PRACTICE
De-Escalating Sepsis
By Francella Crespo, MSN, CCRN, RN-BC, WTA-C
By Francella Crespo, MSN, CCRN, RN-BC, WTA-C
3 MIN READ

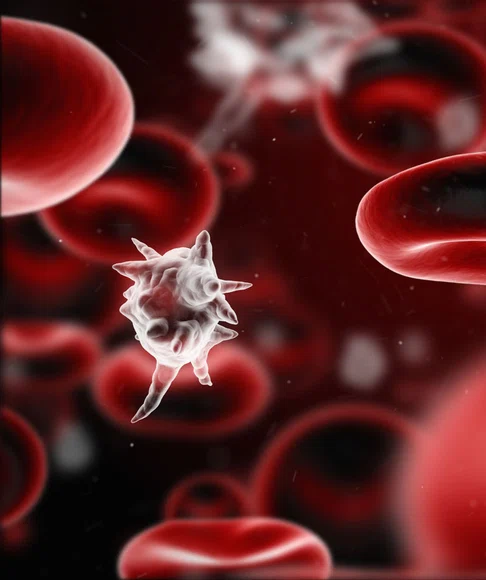
Sepsis is the body’s systemic inflammatory response to an infection that can lead to tissue damage, organ failure, and death (Sepsis Alliance, 2020). The most common infections that trigger sepsis in the adult population occur in the lungs, urinary tract, gut, and skin (CDC, 2020).
Frequently, hospitals admit patients experiencing one of the Sepsis Pathways: Systemic Inflammatory Response Syndrome (SIRS), Sepsis, Severe Sepsis, or Septic Shock. Understanding the development of sepsis and recognizing incidents that lead to septic shock will result in the identification of symptoms and improve patient outcomes. The more knowledge we have, the quicker we can readily identify triggers that escalate this condition.
Sepsis begins with a systemic inflammatory response and presents with two of the following symptoms:
- Hyperthermia (temperature >100.9°F)
- Hypothermia (temperature < 96.8° F)
- Tachycardia (heart rate > 90 beats per minute)
- Tachypnea (respirations > 20 breaths per minute)
- White blood cell (WBC) count >12,000 or < 4,000
- Normal WBC with >10% bands.
The presence of a suspected or confirmed infection with two of the symptoms listed above is considered Sepsis. When the infection begins to affect organs, Sepsis becomes Severe Sepsis. Lungs begin to require more oxygen. The brain is affected and mental status declines, often displaying acute changes such as confusion or lethargy. The cardiovascular system is affected, and blood pressure may decrease with systolic blood pressure less than 90mmHg and mean arterial pressure (MAP) less than 65 mmHg. Lactic acid accumulation in the blood occurs when the body has a high demand for energy without an adequate supply of oxygen. With Severe Sepsis, lactic acid levels are usually elevated above 2.0 mmol/L. Additionally, the liver may fail to clean the blood system of bilirubin resulting in an elevated bilirubin level of greater than 2.0mg/dL. Kidneys are also affected, which is evident with elevated creatinine levels greater than 2.0 mg/dL. Poor kidney function can also cause urine output reduction resulting in urine output of less than 0.5mL/kg/hr. Lastly, Sepsis causes dysregulation of the hemostatic system, and there is an increased risk for bleeding usually presenting with an INR greater than 1.5, a PTT greater than 60 seconds, or platelet count less than 100,000 (Sepsis Alliance, 2020).
Time is the best tool available when treating sepsis. Early recognition with identification of symptoms is important in patients who develop this condition. A thorough nursing assessment can prevent an escalation of infection responses by monitoring of patient symptoms. Familiarity with signs of organ dysfunction and evaluation of a patient’s co-morbidities can likewise aid in distinguishing between sepsis and other health issues. Sepsis and the body’s reactive inflammatory response are extremely taxing on the body’s resources.
References:
Centers for Disease Control and Prevention. (2016). Making Health Care safer. Think Sepsis. Time Matters. Retrieved August 7, 2022, from https://www.cdc.gov/vitalsigns/sepsis/
Related Articles

EDUCATION
Strengthen Your Assessment Skills With Elsevier Clinical Skills

NURSING SCIENCE
Methodist Proficient Assessment CompetencyTM (MPAC) in 2023
Contact us at CNREPHelp@houstonmethodist.org
Questions or comments?
© 2022. Houston Methodist, Houston, TX. All rights reserved.










