Recent Research Review
6 MIN READ

NURSING SCIENCE

Title:
Needleless connector decontamination for prevention of central venous access device infection: A pilot randomized control trial Published: February 2021 in American Journal of Infection Control
Level of Evidence:
Level B
What was the purpose?
This study compared three different needleless connector decontamination products in what was termed a pilot study. A pilot study is usually undertaken to understand better how the study's components work together and identify issues that could influence outcomes. Pilot studies often have sample sizes that are too small to detect significant differences (Morin, 2013).
What was the population studied?
The researchers studied 180 patients who were 18 years of age or older; had a Central Venous Access Device (CVAD), which was either a peripherally inserted or a tunneled, cuffed central catheter, inserted less than 24 hours prior to enrollment; CVAD required for seven days or more, and able to provide written consent. While the initial sample size was 180, only 178 patients were analyzed due to two instances of CVAD insertion failure.
Was the setting similar to Houston Methodist? Were the patients comparable to our patients?
The two institutions involved were identified and not described, so it was difficult to tell how similar they were to Houston Methodist Hospital. The sample patients were described in terms of: age, admission type, number of comorbidities, whether they were receiving cancer treatment, had leucocytes less than 500/µl or pre-existing infection, the type of device, number of lumens and locations, and type of IV medications received. Further discussion of the reason for CVAD Placement and specific pre-existing conditions may have lent additional clarity. Subsequent studies may benefit from including factors such as acuity, specific pre-existing conditions, or risk factors increasing the potential for infection.
Did they use appropriate methods?
The investigators utilized centralized, computer-generated randomization for the study patients. Statistics were analyzed using the Research Electronic Data Capture (REDCap, Nashville, TN) and Stata 15 (College Station, TX). Protocol adherence and RN satisfaction were determined from RN surveys. The inherent subjectivity of survey data may be a study limitation.
What were their findings?
The authors reported high values for eligibility, retention, protocol adherence, missing data, and RN satisfaction which were their protocol feasibility factors. The incidence of central line-associated infection was 2% in both groups using only 70% alcohol (wipes and caps) and 0% in the 2% CHG + 70% alcohol (wipes). The authors acknowledged that a larger randomized controlled trial would be needed to differentiate these outcomes significantly.
Do their findings make sense?
The reported findings make sense. Concerning the incidence of CLABSI, the authors indicated they appeared to be consistent with other investigations looking at the combination of CHG and alcohol.
Examination of this study also prompts additional questions to be explored in future studies. Some examples include:
- Would infection rates differ between a peripherally inserted central catheter (PICC) vs. a central venous access device (CVAD)? This study keeps these two types of catheters labeled as one versus separating them.
- Could further recruitment of participants exhibit different findings? Patient characteristics are widespread. For a more specific study, inclusion and exclusion criteria could be tightened.
- The reported dwell times for the various catheters vary between 7.4-11.3 days. In a study that lasted only four weeks, this variation in time may be clinically significant. How could this variation be decreased? Also, would the results have been different if the CVAD dwell times had been longer?
- Should certain risk factors (i.e., underlying conditions, immunosuppression, current infection at the time of insertion) be controlled to minimize variation or potential additional causes for CLABSI?
- Should the indication for CVAD placement be similar at the time of insertion?
- Did any other care of the patient with the CVAD change? Were all patients following the same protocols for dressing changes, tubing changes, blood draws, etc.?
- Would results have been different if only one type of needleless connector device was used?
- The investigators report that recent data has shown no differences in effectiveness between 5, 10, or 15 second scrub times in the discussion section. While the nurses reported following the manufacturer's recommendations, does this additional variable alter results?
How did things change?
This study did not report any changes in standard of practice in either of the participating hospitals; that was not its purpose. However, the study did add to the evidence on which clinicians may base proposals for practice change. The researchers made suggestions for further research to compare these various products' efficacy to improve best practices as needed.
How is this important for nursing?
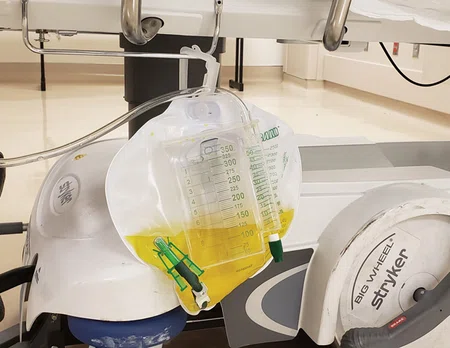
CLABSI prevention remains a hallmark of nursing care. As hospitals increase morbidity, mortality, and hospital lengths of stays, nurses are regularly challenged with maintaining central line maintenance bundles. As products continue to advance and offer reported "better protection," nurses are tasked with staying current in evidence-based practice and critically critiquing any new products or procedures. Since CLABSI prevention is an essential issue at Houston Methodist, perhaps a randomized controlled trial should be conducted here.
To read the entire article, click here.
To read the entire article, click
here
.References:
Morin, Karen H, DSN, RN, FAAN, ANEF (2013). Value of a pilot study. Journal of Nursing Education, 52(10), 547-548. doi: http://dx.doi.org/10.3928/01484834-20130920-10
Related Articles

NURSING SCIENCE
Randomized Controlled Trials—Why Are They the Gold Standard?
PROFESSIONAL DEVELOPMENT
Preventing CAUTIs & CLABSIs: Putting Evidence into Practice
Contact us at CNREPHelp@houstonmethodist.org
Questions or comments?
© 2021. Houston Methodist, Houston, TX. All rights reserved.










